Introduction
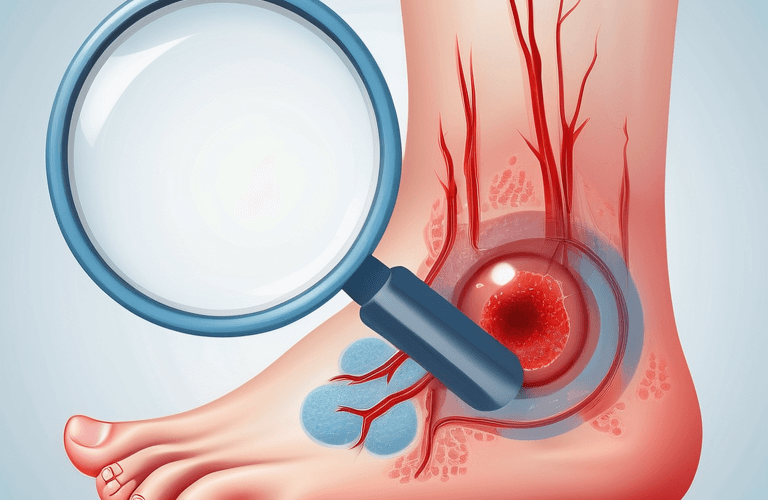
Diabetic foot ulcers are a common and potentially debilitating complication of diabetes. They occur in around 15% of people with diabetes and can lead to serious health complications if left untreated. Diabetic foot ulcers are open sores or wounds that usually develop on the feet, particularly on the balls of the feet, under the big toe, or on the metatarsals. They can be caused by various factors, including injury, poor circulation, nerve damage (neuropathy), and foot deformities.
The severity of diabetic foot ulcers should not be underestimated. If left untreated, they can lead to infection, gangrene (tissue death), and may even require amputation. However, with early detection, proper treatment, and preventive measures, the risks and complications associated with diabetic foot ulcers can be minimized.
In this comprehensive guide, we will delve into the world of diabetic foot ulcers, exploring their causes, signs, stages, risk factors, preventive measures, treatment options, and the vital role of healthcare professionals in managing this condition. We will provide you with the knowledge and tools you need to understand and take care of your feet if you have diabetes. So let’s dive in and learn all about the 7 deadly signs of diabetic foot ulcers.
Understanding Diabetic Foot Ulcers
Diabetic foot ulcers are a common complication of diabetes mellitus, a chronic metabolic disorder characterized by high blood sugar levels. These ulcers are open sores or wounds that typically develop on the feet, particularly in areas of high pressure or friction. They can be caused by a combination of factors, including poor circulation, nerve damage (neuropathy), and foot deformities. Diabetic foot ulcers require prompt medical attention and proper management to prevent complications and promote healing.
The Basics of Diabetic Foot Ulcers
Proper foot care is essential for individuals with diabetes to prevent the development of diabetic foot ulcers. Diabetic neuropathy, a condition characterized by nerve damage, is a common complication of diabetes that can lead to numbness or tingling in the feet. This loss of sensation can make it difficult for individuals to detect injuries or abnormalities in their feet, increasing the risk of foot ulcers.
In addition to nerve damage, poor circulation, often caused by peripheral artery disease, can impair blood flow to the feet. This reduced blood flow can slow down the healing process, making it more difficult for foot ulcers to heal. Individuals with diabetes should pay close attention to their foot health and take steps to improve blood flow, such as exercising regularly and avoiding smoking.
Maintaining good blood sugar control is also crucial in preventing diabetic foot ulcers. High blood sugar levels can impair the immune system’s ability to fight infections and slow down the healing process, putting individuals at a higher risk of developing foot ulcers. Regular monitoring of blood sugar levels and adherence to diabetes management plans are vital components of foot ulcer prevention.
Why Diabetic Foot Ulcers Are a Major Concern
Diabetic foot ulcers are a major concern due to their potential to cause serious health complications and significantly impact a person’s quality of life. If left untreated, foot ulcers can lead to infection, which can spread to the bones and other tissues, resulting in cellulitis, abscesses, or even sepsis. These infections can be difficult to treat and may require prolonged medical care, including antibiotics and wound debridement.
The healing process for diabetic foot ulcers can be slow and complicated. Poor circulation, nerve damage, and impaired immune function can all contribute to delayed healing and increase the risk of complications. In severe cases, diabetic foot ulcers can lead to gangrene, a condition characterized by tissue death, which may necessitate amputation to prevent the spread of infection.
Diabetic foot ulcers also have a significant economic impact, as they often require frequent medical visits, specialized wound care, and prolonged hospital stays. Prevention and early intervention are essential in reducing the burden of diabetic foot ulcers and improving patient outcomes.
Identifying the Signs of Diabetic Foot Ulcers
Diabetic foot ulcers can manifest in various ways, making early identification crucial. Common signs include persistent numbness or tingling in the affected area. Additionally, diabetic ulcers, characterized by sores that are slow to heal, are a prominent indicator of diabetic foot issues. Keep a close eye on any redness, swelling, or drainage around an ulcer, especially if located on the big toe. These visible indications often signal the need for immediate medical attention to prevent complications like infections or amputations. If you notice any of these signs, consulting a healthcare provider promptly is vital for proper treatment and preventing further progression of the ulcer.
1. Diabetic Ulcers
Diabetic ulcers, a common complication of diabetes, are open sores that typically develop on the feet due to poor circulation and nerve damage. These ulcers are often painless initially, making them easy to overlook. People with diabetic ulcers are at high risk of infections and other severe complications, potentially leading to lower extremity amputations. It is crucial for individuals with diabetes to inspect their feet daily for any signs of ulcers, including redness, swelling, or drainage. Prompt treatment by a healthcare provider is essential to prevent further progression of the ulcers and promote healing. Proper wound care, antibiotics, and offloading pressure from the affected area are typical management strategies for diabetic ulcers.
2. Numbness or Tingling
Numbness or tingling in the feet is a common sign of diabetic neuropathy, linked to high blood sugar levels. This results from impaired blood flow to peripheral nerves due to vascular conditions. In diabetic foot ulcers, numbness can delay injury detection. Promptly addressing numbness is crucial to prevent severe nerve damage and complications like amputation. Monitoring for these sensations is vital for early intervention in diabetic foot disease.
3. Changes in Skin Color
Changes in skin color in diabetic foot ulcers can indicate important issues. Redness may signal infection-related inflammation, while a pale or bluish tone could suggest reduced blood flow, potentially due to peripheral artery disease. Monitoring these color changes is crucial for understanding ulcer progression and complications. Prompt medical attention is vital for any unusual discoloration around the ulcer to prevent severe outcomes like amputation. Early recognition of these visual cues can aid in proper treatment, healing, and reducing complication risks. Be vigilant for skin color changes as a warning sign that needs immediate attention.
4. Swelling
Swelling in diabetic foot ulcers is a common symptom caused by inflammation and impaired blood flow, leading to increased pain and infection risk. Monitoring for unusual swelling is crucial as it may indicate ulcer progression or vascular issues. Severe swelling can hinder healing and elevate amputation risks. Timely intervention and treatment are vital. Consult a healthcare provider promptly if you observe significant swelling or ulcer size changes.
5. Increased Temperature
Elevated temperatures in diabetic foot ulcers can indicate the presence of inflammation, infection, or other complications. This heightened temperature is often a response to pathogens and should not be ignored. When coupled with symptoms such as redness, swelling, and drainage, it is imperative to seek immediate medical assistance. Regular monitoring of temperature levels in diabetic foot care is essential for the timely identification of issues and prompt initiation of treatment to prevent further complications and promote healing. Early detection through temperature checks can significantly improve outcomes for individuals managing diabetic foot ulcers and aid in maintaining overall foot health.
6. Foul Smelling Discharge
Individuals with diabetic foot ulcers should watch for foul-smelling discharge, a sign of infection. Immediate medical attention is crucial to prevent complications. Monitoring for redness, warmth, swelling, or pain is also important. Proper wound care and blood sugar control are essential to prevent infections and promote healing. Regular foot exams can help detect issues early and avoid serious consequences.
7. Gangrene
Gangrene, a severe complication of diabetic foot ulcers, results from infections and poor blood circulation. It can lead to tissue death and lower extremity amputation if not promptly treated. Peripheral artery disease and diabetic neuropathy contribute to its development. Symptoms include blackened tissue, foul discharge, and extreme pain, requiring immediate medical intervention. Treatment involves podiatrists, vascular surgeons, infectious disease specialists, wound care, and sometimes surgical debridement. Optimal blood sugar control and adherence to treatment are crucial in preventing gangrene.
The Stages of Diabetic Foot Ulcers
Diabetic foot ulcers can be classified into different stages based on their severity and depth. These stages help healthcare professionals assess the condition of the ulcer and determine the appropriate treatment plan. The two most widely used classification systems for diabetic foot ulcers are the University of Texas Diabetic Foot Ulcer System and the Wagner Diabetic Foot Ulcer System. These systems categorize foot ulcers based on various factors, such as wound depth, presence of infection, and presence of ischemia (reduced blood flow).
Early Stages: Recognizing Warning Signs
Early detection of diabetic foot ulcers is crucial in preventing complications and promoting effective treatment. Here’s what you need to know about the early stages and warning signs:
- In the early stages, diabetic foot ulcers may present as minor injuries, such as redness, swelling, or small sores on the feet.
- These warning signs should not be ignored, as they can progress to more severe ulcers if left untreated.
- Regular foot inspections are essential for early detection. Check for any changes in skin color, temperature, sensation, or the presence of wounds or abnormalities.
- Individuals with diabetes should pay close attention to their feet and report any warning signs to their healthcare provider or a podiatrist.
- Managing risk factors, such as poor blood sugar control, poor circulation, and foot deformities, can help prevent the development of foot ulcers.
- Practicing good foot care, including proper hygiene, regular moisturizing, and wearing well-fitting shoes, is essential in reducing the risk of foot ulcers.
By recognizing the warning signs and taking proactive measures, individuals with diabetes can prevent the progression of foot ulcers and minimize the risk of complications.
Advanced Stages: Symptoms and Complications
In the advanced stages of diabetic foot ulcers, the symptoms become more severe, and complications can arise. Here’s what you need to know:
- Advanced stages of diabetic foot ulcers may involve deep wounds, exposed bones or tendons, severe infections, and extensive tissue damage.
- Symptoms can include increased pain, foul smelling discharge, difficulty walking, and difficulty healing.
- Complications can include cellulitis, osteomyelitis (bone infection), sepsis, and the potential need for amputation.
- Prompt medical care is crucial in managing advanced diabetic foot ulcers. Healthcare professionals may recommend wound debridement, antibiotics, off-loading techniques, and other specialized interventions.
- Multidisciplinary care, involving a team of healthcare professionals, is often necessary to provide comprehensive treatment and address the various aspects of the condition.
- Individuals with advanced diabetic foot ulcers should closely follow their healthcare provider’s guidance and attend regular follow-up appointments to monitor the progress of healing and address any complications.
Effective management and timely intervention can help improve outcomes and reduce the risk of further complications in individuals with advanced diabetic foot ulcers.
Preventive Measures to Avoid Diabetic Foot Ulcers
Preventive care is essential in reducing the risk of diabetic foot ulcers. Here are some key preventive measures:
- Regular foot inspections: Check your feet daily for any signs of injury, redness, swelling, or abnormalities.
- Proper foot care: Keep your feet clean and dry, moisturize regularly, and trim your toenails carefully.
- Importance of proper footwear: Wear well-fitting, supportive shoes that protect your feet and reduce the risk of friction or pressure points.
- Managing blood sugar levels effectively: Monitor your blood sugar levels regularly, follow your diabetes management plan, and work closely with your healthcare team.
- Regular check-ups with healthcare providers: Schedule regular foot examinations with a podiatrist or diabetes specialist to assess your foot health and address any concerns.
By incorporating these preventive measures into your daily routine and diabetes management plan, you can significantly reduce the risk of developing diabetic foot ulcers and their associated complications.
Regular Foot Inspections and Care
Regular foot inspections and care are crucial in preventing diabetic foot ulcers. Here’s what you need to know:
- Perform daily foot inspections: Check your feet thoroughly for any signs of injuries, cuts, redness, swelling, or changes in skin color or temperature.
- Use a mirror or ask for assistance if you have difficulty seeing the soles of your feet.
- Practice proper foot hygiene: Wash your feet daily with lukewarm water and mild soap, pat them dry gently, and moisturize with a diabetic-friendly lotion.
- Trim your toenails carefully: Cut them straight across and file any sharp edges to prevent ingrown nails and injuries.
- Avoid self-treatment of foot problems: If you notice any abnormalities or concerns, seek professional advice from a podiatrist or healthcare provider specializing in diabetes.
- Follow your healthcare provider’s recommendations: Attend regular check-ups, discuss any foot concerns or changes, and adhere to their instructions and treatment plans.
Regular foot inspections and care, coupled with professional guidance, can help detect and address any potential issues early on, reducing the risk of diabetic foot ulcers.
Importance of Proper Footwear
Proper footwear plays a crucial role in preventing diabetic foot ulcers. Here’s why it’s important:
- Choose well-fitting shoes: Wear shoes that provide ample room for your toes, have a wide toe box, and offer proper arch support and cushioning.
- Avoid tight or loose shoes: Ill-fitting shoes can cause pressure points, friction, and blisters.
- Protect your feet: Wear shoes that cover and protect your entire foot, reducing the risk of injuries.
- Select appropriate socks: Opt for seamless, moisture-wicking socks that fit well and help keep your feet dry.
- Inspect your shoes regularly: Check for any signs of wear and tear, loose stitching, or foreign objects that could cause discomfort or injury.
- Replace worn-out shoes: Replace your shoes when they show signs of wear or after a certain period, as recommended by your healthcare provider.
Proper footwear, combined with regular foot inspections and care, can significantly reduce the risk of foot ulcers and promote foot health in individuals with diabetes.
Managing Blood Sugar Levels Effectively
Managing blood sugar levels effectively is crucial in preventing diabetic foot ulcers. Here’s what you need to know:
- Monitor your blood sugar levels regularly: Use a blood glucose monitor as directed by your healthcare provider and keep track of your readings.
- Follow your diabetes management plan: Take your prescribed medications, insulin injections, or use other glucose-lowering treatments as recommended.
- Maintain a healthy diet: Eat a balanced diet rich in whole grains, lean proteins, fruits, vegetables, and healthy fats, and limit your intake of sugary or high-carbohydrate foods.
- Engage in regular physical activity: Exercise regularly to help control blood sugar levels, improve circulation, and maintain a healthy weight.
- Work closely with your healthcare team: Attend regular check-ups, discuss any concerns or changes in your diabetes management, and follow their recommendations for blood sugar control and foot care.
By effectively managing your blood sugar levels, you can reduce the risk of complications associated with diabetes, including diabetic foot ulcers.
Living with Diabetic Foot Ulcers
Living with diabetic foot ulcers can be challenging, but there are lifestyle modifications and coping strategies that can improve quality of life. Some tips for living with diabetic foot ulcers include:
- Proper foot care: Regularly inspecting the feet, keeping them clean and moisturized, and wearing appropriate footwear.
- Following a healthy diet: Eating a balanced diet rich in fruits, vegetables, lean proteins, and whole grains can promote healing and overall health.
- Managing blood sugar levels: Keeping blood sugar levels within target range through medication, diet, and exercise can help prevent complications and promote healing.
- Seeking support: Connecting with support groups or healthcare professionals who specialize in diabetic foot ulcers can provide valuable information and emotional support.
- By incorporating these lifestyle modifications and coping strategies into daily life, individuals with diabetic foot ulcers can improve their overall well-being and better manage their condition.
Lifestyle Modifications and Coping Strategies
Making lifestyle modifications and implementing coping strategies can significantly improve the management of diabetic foot ulcers. Some lifestyle modifications and coping strategies to consider include:
- Making healthy dietary changes: A balanced diet rich in whole foods, fruits, vegetables, and lean proteins can support healing and overall health.
- Engaging in regular physical activity: Physical activity can improve blood circulation, promote healing, and help manage blood sugar levels.
- Practicing proper foot care: Regularly inspecting the feet, keeping them clean and moisturized, and wearing appropriate footwear can prevent complications and promote healing.
- Managing stress and mental health: Stress can impact blood sugar levels and overall well-being. Engaging in stress-reducing activities such as yoga, meditation, or talking to a therapist can be beneficial.
- Seeking support: Connecting with support groups or healthcare professionals who specialize in diabetic foot ulcers can provide valuable information and emotional support.
- By incorporating these lifestyle modifications and coping strategies into daily life, individuals can better manage their diabetic foot ulcers and improve their overall well-being.
Conclusion
In conclusion, understanding diabetic foot ulcers is crucial for effective management and prevention. These ulcers pose a significant risk, especially for individuals with diabetes, due to complications like peripheral artery disease and neuropathy. By recognizing the 7 Deadly Diabetic Foot Ulcer Signs early on, individuals can seek timely medical intervention, reducing the likelihood of severe outcomes such as lower extremity amputations. It’s imperative for healthcare providers to follow clinical practice guidelines and implement appropriate treatment strategies to address diabetic foot disease comprehensively. Lifestyle modifications, regular foot care, and monitoring blood sugar levels are vital in managing diabetic foot ulcers and preventing recurrence. Seeking prompt medical attention at the onset of any foot problems can significantly impact the healing process and overall prognosis. Ultimately, with proper treatment and diligent self-care, individuals can lead fulfilling lives while effectively managing diabetic foot complications.
Frequently Asked Questions
What Are the First Signs of a Diabetic Foot Ulcer?
The first signs of a diabetic foot ulcer may include redness, swelling, or tenderness around a specific area of the foot. Open sores or wounds that are not healing or are getting worse may also be early signs of a diabetic foot ulcer. If you notice any of these signs, it is important to seek medical attention as soon as possible.
Can Diabetic Foot Ulcers Be Completely Healed?
With proper medical treatment, many diabetic foot ulcers can be completely healed. However, the healing process can vary depending on the severity of the ulcer, the individual’s overall health, and their adherence to the treatment plan. It is important to seek medical attention and follow the recommended treatment plan to improve the chances of complete recovery.
What is the last stage of diabetic foot ulcer?
The last stage of a diabetic foot ulcer can vary depending on the severity and extent of the ulcer. In some cases, it may progress to the point where amputation is necessary to prevent the spread of infection or further complications. Regular monitoring and early intervention can help prevent the ulcer from reaching this stage.
When should diabetics go to the ER for foot ulcers?
Individuals with diabetic foot ulcers should go to the emergency room if they experience signs of a serious infection, such as fever, chills, or increased pain. It is also important to seek immediate care if the foot ulcer is accompanied by severe symptoms or if the condition worsens rapidly. Prompt medical attention can help prevent further complications and ensure proper treatment.
Are diabetic foot ulcers serious?
Diabetic foot ulcers are serious as they can lead to severe complications like infections and amputations if not treated promptly. Monitoring signs, seeking medical advice, and following treatment plans are crucial to prevent escalation. Early intervention is key in managing diabetic foot ulcers effectively.